BY: LILY YANG AND NICOLE ARNOLD
Hepatitis A Outbreaks
Should the Hepatitis A vaccine be made mandatory for those working in the food industry? Currently, this question is being posed as Hepatitis A virus (HAV) outbreaks associated with food, water, and other sources have become more publicized in the media. In 2003, at least 565 cases of Hepatitis A were associated with the consumption of contaminated green onions at a restaurant in Pennsylvania. Of these 565 infections, at least 128 people were hospitalized and 3 people died. While contaminated green onions were implicated as the source of the outbreak, and not the restaurant workers – human-to-human contact is another possible mode of contamination – the Hepatitis A immune globulin (aka: the Hepatitis A vaccine) was given to over 9,000 restaurant patrons (along with those who’d been exposed to the ill) (CDC, 2003).

https://images.google.com/imgres?imgurl=https%3A%2F%2Fwww.lcdhd.org%2Fwp-content%2Fuploads%2F2016%2F09%2Fpicture-employee_hand_washing.gif&imgrefurl=https%3A%2F%2Fwww.lcdhd.org%2Fservices%2Fenvironmental%2Fprograms%2Ffood-service%2F&docid=uCEFT2S7SxuTzM&tbnid=5kcgBPE8lHSiCM%3A&vet=1&w=247&h=393&source=sh%2Fx%2Fim
To date, this is one of the largest Hepatitis A outbreaks ever recorded. More recently this past month, two Detroit restaurants were shut down due to Hep A outbreaks associated with their locations (Powell, 2017). When looking globally, there was also a Hepatitis A outbreak linked to lettuce consumption in Australia with 12 individuals falling ill; these cases are associated with a simultaneous 1000-person outbreak in Europe (Brennan, 2017). At this moment, there is an extensive Hepatitis A outbreak/epidemic occurring in California, which has sickened at least 569 individuals and been associated with 17 deaths. This HAV epidemic in California is continuing to spread through much of the homeless communities throughout California, and as the development of symptoms is slow, it is estimated that it will be years before California will have fully recovered from this epidemic (Karlamangla, 2017).
While the proportion of individuals that are identified as acquiring Hepatitis A is relatively low, the World Health Association (2012) estimates that HAV is responsible for half the total number of human hepatitis infections diagnosed yearly worldwide (1.4 million new cases diagnosed yearly). Along with norovirus, HAV is of great food safety concern because of its high level of incidence, disease severity, transmission methodologies, and mortality rate. Despite all of this, there is good news! It is the only preventable foodborne illness – through vaccine – that exists (Sanchez, 2015).
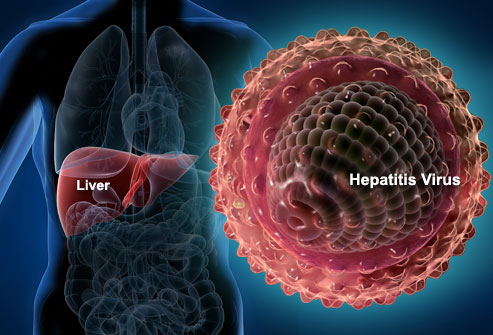
What is Hepatitis A?
When we think of becoming ill via a food source, we oftentimes think of bacteria; however, Hepatitis A causes a viral infection from the Hepatitis A virus (HAV). It is part of a larger set of hepatitis viruses that include other enterovirus groups of the Picornaviridae family that also contain hepatitises B, C, and E. While Hepatitis A is a viral liver disease, it does not have the chronic nor fatal symptoms that is generally associated with a Hep B or C liver disease infection (WHO, 2017). HAV particles, while not able to grow in the environment, can persist with vigor “under a wide range of environmental conditions, including freezing, heat, chemicals, and desiccation”, in addition to many other common sanitizing agents, processes, or cleaning steps. (FDA, 2012; WHO 2017).
Unfortunately, not only is it a hardy organism, like with other foodborne illnesses we’ve discussed in the past, HAV can also be transmitted directly from person-to-person contact or through the fecal-oral route when contaminated food or water is ingested after contact with an infected individual or HAV can also be contracted sexually. HAV has been linked to many different foods/commodities over the years such as berries, lettuce, green onions, shellfish and tuna!

https://images.google.com/imgres?imgurl=https%3A%2F%2Fcbsdetroit.files.wordpress.com%2F2016%2F11%2Fistock_78323185_small.jpg%3Fw%3D640%26h%3D360%26crop%3D1&imgrefurl=http%3A%2F%2Fdetroit.cbslocal.com%2F2016%2F11%2F05%2Fhepatitis-a-outbreak-linked-to-frozen-strawberries-served-at-metro-detroit-businesses-check-the-list%2F&docid=UmucmtSwQ_9YvM&tbnid=YxbZDeJkhlXfKM%3A&vet=1&w=640&h=360&source=sh%2Fx%2Fim
The onset of illness usually begins between 2 – 6 weeks after contact with contaminated food or water but will usually resolve itself within a week or two after symptoms arise, although symptoms can last up to 6 months. Because its incubation period can be lengthy, identifying the specific contaminated food source can often be difficult. During this time, the liver becomes infected and inflamed with the possibility of developing jaundice (yellowing of skin and eye whites), along with the general malaises of fever, low appetite, nausea, vomiting, diarrhea, and/or muscle aches. In rare instances, the more mild flu-like symptoms of HAV can deteriorate rapidly into a deadly acute liver infection from fulminant hepatitis (hepatic disease) with hepatic necrosis, liver failure, and a 75% fatality rate. Luckily, once infected with HAV (or vaccinated, as we’ll discuss), individuals tend to develop lifelong immunity to the virus.

https://images.google.com/imgres?imgurl=http%3A%2F%2Fwww.bestonlinemd.com%2Fwp-content%2Fuploads%2F2017%2F04%2Fhepatitis-A.jpg&imgrefurl=http%3A%2F%2Fwww.bestonlinemd.com%2Fwhat-is-hepatitis-a%2F&docid=MbiF9yswqaQ32M&tbnid=qJRigni-EKGjCM%3A&vet=1&w=600&h=336&source=sh%2Fx%2Fim
Implications of the virus
Outbreaks of HAV, while sporadic, can be very debilitating. Hepatitis A itself does not often cause death; however, the economic, social, and productivity ramifications are devastating. The estimated yearly total cost of HAV infections is now over $50M USD (Sanchez, 2015). And within the food industry, the increased importation and exportation of food products has contributed to the global spread of the virus (Sanchez, 2015). And this is where all the controversy surrounding the Hepatitis A vaccine begins…
What is all the controversy about?
Currently, food businesses do not require the Hepatitis A vaccine for their employees. Although food handlers are in contact with raw foods, employees are typically left to make their own decision whether or not to get vaccinated. Indeed, there seems to be a lack of knowledge regarding Hepatitis A in the food industry. Current discussion revolves around (a) whether food businesses should require their employees to be vaccinated and (b) if said businesses should foot the cost for vaccination. The economic burden of mandatory vaccinations plays a major role in why something seemingly positive nature has not been put into effect across the food industry.
How can I prevent an HAV infection?
Way 1, through food processing:HAV is part of the passively-surveillanced pathogens and is part of the National Notifiable Diseases Surveillance System (NNDSS) (Scallen, 2011). As discussed above, HAV inactivation after contamination is often quite difficult, even through conventional processing and storage techniques. However, oftentimes, cooking food products to an inactivation temperature of 185°F for at least one minute is what is needed to kill the virus in foods (CDC, 2006). So, if you’re at home, make sure to use those thermometers! That said, new technologies, like high pressure processing, have shown promise in inactivating the virus from the production standpoint (Sanchez, 2015).
Way 2, by preventing spread through other people: Some of the most important methods of limiting HAV infections is through decreasing the transmission of HAV between individuals and include what we’ve talked about throughout many of our articles: (a) wash your hands after using the bathroom, possible contact with fecal matter, and before preparing or eating food; (b) immune-globin shots (aka: get vaccinated) [Health, NY]; and (c) don’t touch food with your bare hands. In Alaska, new proposed regulation will have bartenders start using gloves or utensils to make mixed drinks containing lemons, limes, and other garnishments to not only prevent the spread of HAV, but also as a preventative measure against other foodborne illnesses such as norovirus (Kelly, Alaska Dispatch News, 2017).
Conclusion
Ultimately, Hepatitis A is a devastating foodborne illness, but is preventable if proper precautions and hurdles are put in place. So readers, please don’t forget to wash your hands! But, tell us, what are your thoughts on mandating the Hepatitis A vaccine for food industry employees?
Sources:
FDA Bad Bug Book
WHO Media Centre http://www.who.int/mediacentre/factsheets/fs328/en/
http://www.latimes.com/local/california/la-me-ln-hepatitis-outbreaks-20171006-htmlstory.html
https://www.niddk.nih.gov/health-information/liver-disease/viral-hepatitis/hepatitis-a
http://www.barfblog.com/2017/09/hepatitis-a-transmission-door-knob-edition/ [doorknobs]
https://www.fda.gov/food/recallsoutbreaksemergencies/outbreaks/ucm561199.htm [Tuna]
“Foodborne Illness Acquired in the United States – Major Pathogens” Scallen et al., 2011.
https://www.health.ny.gov/diseases/communicable/hepatitis/hepatitis_a/food_service_workers_fact_sheet.htm (Health NY)
http://onlinelibrary.wiley.com/doi/10.1111/1541-4337.12154/full
-
- http://www.latimes.com/local/california/la-me-ln-hepatitis-outbreaks-20171006-htmlstory.html (below)
- http://www.barfblog.com/2017/08/restaurant-employee-positive-for-hepatitis-a/ (should discuss)
- https://www.adn.com/alaska-news/anchorage/2017/08/29/gloves-for-bartenders-anchorage-proposes-updates-to-local-food-safety-laws/
- http://www.barfblog.com/2017/09/food-safety-broken-telephone-or-is-someone-really-testing-food-for-hepatitis-a/
- http://onlinelibrary.wiley.com/doi/10.1111/1541-4337.12154/full
Powell, D. 2017. Barfblog. http://www.barfblog.com/2017/10/2-detroit-restaurants-close-during-hepatitis-a-probe/
Brennan (2017). Lettuce link to Sydney hepatitis A outbreak with 12 new cases. http://www.news.com.au/national/nsw-act/sydney-hit-by-hepatitis-a-outbreak-with-12-news-cases/news-story/ebcaeb265a78a4b03e7df5d274a7db85
https://www.cdc.gov/mmwr/preview/mmwrhtml/mm52d1121a1.htm
CDC, 2006. https://www.cdc.gov/mmwr/preview/mmwrhtml/rr5507a1.htm





Leave a Reply